Abstract
Treatment of the lower face is a necessary component of an integrated approach to facial rejuvenation. Neurotoxin injections are a cornerstone of addressing age-related changes to the lower face. A knowledge of potential neurotoxin targets provides a foundation for addressing rhytids as well as modifying the overall facial shape. However, the relatively complex muscular anatomy and crucial functional roles of the lower face can result in an increased rate of complications. The following text is organized in a brief, problem-based approach with accompanying video demonstrations of the techniques discussed.
Introduction
A complex interplay of dynamic physiologic and structural anatomic factors contribute to facial aging.1,2 Owing in part to gravitational force, the lower face becomes the focal point of many of age-related changes. These changes may be particularly noticeable given the central role of the lower face verbal and non-verbal communication, as well as the significant importance of the smile and an emphasis on photography in many Western cultures. As a result, neurotoxin injections into the lower face have increased in popularity over the past twenty years.
In comparison to the upper face, neurotoxin treatment of the lower face presents a particular challenge to the aesthetic practitioner, as the target muscle anatomy is not only more complex, but also plays a role in crucial functions including speech, feeding, mastication, and general expressivity.3 The complication rate of lower face chemodenervation is therefore unsurprisingly higher.3,4 Furthermore, the goals of lower face neurotoxin injections are nuanced, as subtle effects on movement – rather than complete paralysis as in the case of the glabellar complex – may be preferable. Herein, we focus solely on techniques and strategies for safe injection of neurotoxin in the lower face.
Dose recommendations are approximate and must be tailored to an individual patient’s needs, including baseline muscle activity, strength of contraction, gender, and potential natural asymmetries. All patients should undergo a thorough evaluation – with reasonable expectations set and potential complications discussed – prior to treatment.
Injection of the Depressor Anguli Oris: Marionette Lines, Perpetual Frown, and Jowls
Problem & Desired Outcomes:
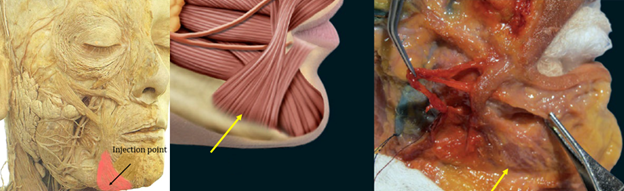
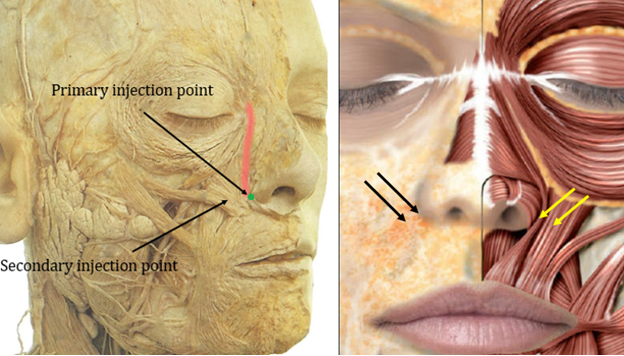
The depressor anguli oris (DAO) is a variably sized muscle with a broader region at its inferior, mandibular attachment.3 Superiorly, the narrow end of the DAO attaches to the modiolus, lateral to the oral commissure.5 Its contraction results in downward traction on the oral commissure and a frowning appearance. Repeated use and time result in vertical creases framing the chin known as marionette lines and the appearance of a perpetual frown known by various colloquialisms. By injecting neurotoxin accurately into the DAO, marionette lines can be softened and the downward slanting appearance of the corners of the mouth reduced (Figure 1).

Injection Sites & Surface Anatomy:
Localization of injection sites is important to avoid inadvertent chemodenervation of nearby muscles of facial expression. In this area, the objective is to avoid diffusion of toxin to the depressor labii inferioris (DLI), orbicularis oris, or modiolus. This can be accomplished by targeting the thicker, inferior portion of the DAO closer to its mandibular insertion (Figure 2). In general, the DAO is found directly below and slightly lateral to the marionette line.3 However, for purposes of confirmation, the muscle belly is readily palpable. Palpation can be aided by telling the patient to grimace, show their lower teeth, or say the letter “E.” Another anatomic structure, the mandibular ligament, can be felt as a subtle cord directly lateral to the DAO. Injection sites should be located into the palpable, lower portion of the DAO 2-3 millimeters medial to the mandibular ligament. Injections should be kept away from the oral commissures (at least 1cm inferiorly and laterally) and care should be taken to avoid injection medial to the DAO to avoid the DLI.
Dose: Doses of 3-5 units of onabotulinum or incobotulinum or 9-15 units of abobotulinum are typically sufficient to result in appropriate chemodenervation.6 Unless deemed necessary, higher doses of neurotoxin may increase the risk of diffusion and complications as described below.
Potential Complications:
Several additional muscles, many with functional importance, insert at the modiolus. These include the buccinator, orbicularis oris, risorius, zygomaticus major, levator anguli oris, and levator labii superioris. For this reason, injection away from this crucial juncture is recommended. Diffusion to the orbicularis oris can abrogate its necessary sphincteric action, resulting in decreased oral competency, difficulty with drinking or retaining water (particularly from a straw), whistling, or articulation. Weakening of buccinator function can result in an inability to chew while temporary paralysis of the zygomaticus, risorius, or levator anguli oris can result in a crooked smile. If injections are to be attempted to the superior portion of the DAO, they should be kept superficial (resulting in skin blebs) and at a maximal allowable distance from the oral commissure.
Injection medial to the DAO can result in chemodenervation of the DLI. Temporary paralysis of the DLI can result in crooked lips, as the normal depressor function of this muscle is abrogated. The resultant uneven appearance is visible at rest but may be accentuated upon speaking or smiling (Figure 3). Speech function, particularly with “O,” “U,” and “W,” phonetics may be altered.7 In these situations, the risks and benefits of corrective contralateral injections should be weighed.

Video Demonstration:
Smoker’s Lines, Lip Softening, and Lip Flip: Injection of the Orbicularis Oris
Problem & Desired Outcomes: Conceptually, the orbicularis oris appears to be a circumferential muscle surrounding the lips, with contraction resulting in sphincter-like actions that allow for pursing of the lips. Strictly speaking however, the orbicularis oris consists of a superior and an inferior component, which each attach to the modiolus to surround the mouth. These components themselves are divided into a pars marginalis (attachment at the vermillion lip with compressive, sphincter function) and pars peripheralis (located within the cutaneous lip with dilative function).3 The combined action of the pars marginalis and peripheralis results in pursing. Repeated contraction results in rhytids radiating perpendicularly to the vermillion known as smoker’s lines. A reduction in dynamic wrinkling and softening appearance can be achieved with chemodenervation of the orbicularis oris. As a result of the aforementioned anatomy, selective inhibition of the compressive function of the pars marginalis by injection of neurotoxin at the vermillion border may result in proportionately greater action of the dilatory pars peripheralis, and thereby explain the eversion of the mucosal lip seen with this technique – also called the “lip-flip.” (Figure 4)

Injection Sites & Surface Anatomy:
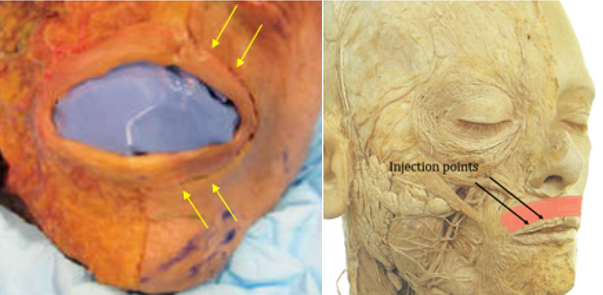
Attachment of the orbicularis oris at the location of the vermillion makes identification of injection sites reliable. Injections are placed superficially below the dermis a few millimeters beyond the vermillion border to avoid accidental chemodenervation of underlying perioral musculature. Laterally displaced injections near the commissures should be avoided, as these may result in inadvertent diffusion of neurotoxin to the modiolus-attached muscles (see above). Midline injections at or within the philthral ridges may result in flattening of the Cupid’s bow. As a result, two injections per side between these lateral and medial boundaries are performed on the upper lip (Figure 5 & 6). Particular attention should be paid to the symmetry of injection sites.
Consideration should be given to injection of the inferior component of the orbicularis oris. The benefit of treating both the upper and lower orbicularis oris is a more uniform effect on the movement of the upper and lower lip, as patients in whom only the upper orbicularis is treated are still able to purse their lower lips. On the other hand, chemodenervation of the lower orbicularis more has a higher potential for adverse effects. First, in comparison to the upper orbicularis, loss of function of the lower orbicularis more frequently results in a functional deficit in eating, drinking, or speaking (see below). Second, the inferior orbicularis injection points lie in close proximity to the DLI, and from a practical perspective inadvertent chemodenervation of this muscle can occur. Third, perioral wrinkles tend to be less pronounced on the inferior cutaneous lip and may be camouflaged by the shadow of the lips superiorly and the concave mental crease inferiorly, lessening the overall impact of neurotoxin injections. Taken together, it is not unreasonable to defer treatment of the lower orbicularis oris.
Dose: Low doses of neurotoxin are recommended to avoid overcorrection. 4U of onabotulinum toxin injected into the upper lip is a safe starting point though 6U is often necessary for optimal effectiveness. If the lower orbicularis is to be treated, 2-3U will typically suffice.
Potential Complications:
The orbicularis is involved in the necessary functions of speech and eating. As such, there is a notable risk of temporary functional deficit with chemodenervation. Overcorrection or near-complete paralysis may result in stiffness of the cutaneous lip and subsequent difficulties with enunciation, chewing, spitting, drinking from a straw or cup, kissing, and other actions which require pursing (Figure 7). As many patients with desirable aesthetic results may experience some degree of functional change, all patients should be counseled on the potential for functional changes and lip incontinence prior to procedure. A notable portion of patients do not tolerate even minor functional alterations.

The relative size of the orbicularis oris and the low doses of toxin administered at each injection site inherently predispose this location to chemodenervation-related asymmetry. Given the central role of the lips in communication, asymmetry from imprecise injection sites may be noticeable by the patient as well as others. Finally, injection sites placed too far laterally may result in central protrusion – “beaking” – of the lips. Fortunately, given the frequency of use of the orbicularis in vital daily functions, chemodenervation of this muscle is relatively short lived and complications reverse more rapidly than other areas of the face.
Video Demonstration:
Gummy Smile: Levator Labii Superioris Alaeque Nasi, Levator Labii Superioris, Zygomaticus Minor
Problem & Desired Outcomes:
While the lips are physically at the center of the face, the smile and appearance of the teeth are at the center of the animated face and smile. Dissatisfaction with appearance may be accentuated by the static nature of photographs. Gummy smile is an imprecise term referring to visibility of the gingiva upon smiling. This is the result of cephalocaudally oriented tension vectors from muscles of facial expression with attachments to the soft tissues of the lip. An incisoral smile, canine smile, or zygomatic smile can result from superior pull on the upper lip from various muscles of the upper-, mid-, and lower-face. These are categorized imprecisely by the predominant areas of maxillary gingival show, from most anteromedial (incisoral smile) to posterolateral (zygomatic smile).
Herein, our discussion of treatment of the gummy smile is limited to addressing visibility of the maxillary gingiva. An example of the improvement that can be obtained via neurotoxin injection is pictured in Figure 8. While inferior pull on the lower lip from an overactive platysma, mentalis, DAO, and buccinators can result in a downturned smile, this must be extreme to result in visibility of the lower gingiva.8 Chemodenervation of the latter muscles of facial expression is discussed elsewhere in this chapter.

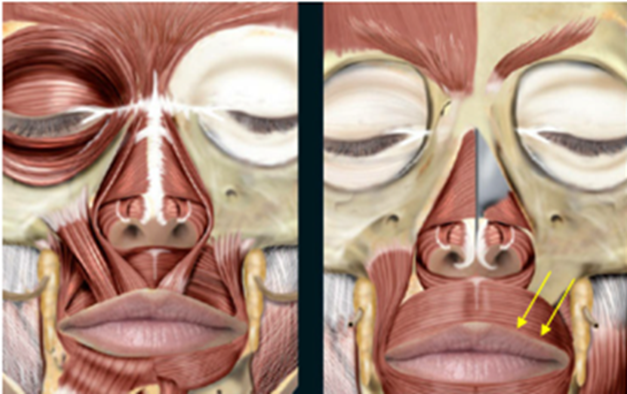
Target muscles of facial expression for neurotoxin-based treatment of the gummy smile include the levatorlabii superioris alaeque nasi (LLSAN), levator labii superioris (LLS), depressor septi, zygomaticus major and zygomaticus minor (Figure 9).
The LLSAN is the central target for addressing a pronounced gummy smile.9 Importantly, chemodenervation of the LLSAN produces predictable results. The LLSAN runs from its origin at the frontal process of the maxilla near the superior nasal sidewall to attachments in the cutaneous tissues of both the nostril (notably resulting in “bunny lines”) and the upper lip. The latter attachment results in its primary role in causing the gummy smile.9 The inferolateral fibers of the LLSAN connect with the fibers of the deeper LLS lateral to the nostril potentially explaining its crucial role in anteromedial gummy smiles as well as the efficacy of targeting the LLSAN.3 Treating the LLSAN with neurotoxin results in decreased upward traction on the upper lip, subsequent lengthening of the upper lip, and ultimately decreased visibility of the maxillary gingiva.
Medial to the LLSAN, the depressor septi nasi muscle travels from its attachment at the incisive fossa of the maxilla to the nasal septum, resulting in a decreased distance between the nasal tip and vermillion lip with contraction. Therefore, it represents an adjunctive target in centrally-dominant gummy smiles.
As chemodenervation of the zygomaticus major and minor results in a generally less aesthetic laterally downturned smile, this is generally utilized only for significant cases of posterolateral gummy – i.e. “Joker” or “Mona Lisa” – smile. Nevertheless, neurotoxin represents a less invasive approach for correction of a joker smile than orthognathic surgery and is advocated by some for correction of a zygomatic dominant Mona Lisa smile.8,10
Injection Sites & Surface Anatomy:
The inferior portion of the LLSAN can be reliably treated with injections into the region of the pyriform aperture or 1-2mm lateral to the middle of the lateral alar groove. Given the interlacing of LLSAN and LLS fibers in this area, injection here is suitable for anteromedial-dominant gummy smiles. Should targeting the LLS be desired, an additional injection 2mm lateral to the LLSAN injection point can be performed, though anatomic studies demonstrate the presence of the zygomaticus in this area.11 Given a potential overlap of all 3 muscles, knowledge of this injection point is valuable for pronounced gummy smiles that include both anteromedial and posterolateral components (Figure 10)
Dose:
1-2 U of onabotulinum toxin or 3-6 U of abonotulinum are approximate starting points to consider for treatment of the LLSAN. Particular attention should be paid to dosage when addressing the gummy smile to account for a high rate of natural asymmetry. Ipsilateral LLSAN doses must commonly be decreased to account for a less pronounced gingival show. When targeted specifically, the LLS and zygomaticus may require 1-4 U and 1-3 U of onabotulinum toxin or equivalent, respectively.3,6 More concentrated reconstitutions of neurotoxin in these areas can be considered to reduce the amount of toxin spread.
Potential Complications:
A notable complication of LLSAN injection is overcorrection resulting in aesthetically displeasing lengthening of the upper cutaneous lip (Figure 11). Because lengthening occurs in all patients (and is necessary to reduce gingival visibility), this possibility should be reviewed prior to injection as there is no quick-fix for this occurrence. Additionally, asymmetric under- or over-correction of the gummy smile is a common complication. Symmetry can be achieved by injection of additional neurotoxin to the relatively undertreated side.

As discussed above, a laterally downturned smile can occur with treatment of the zygomaticus muscles. As such, careful patient selection and counseling is imperative. Accidental unilateral injection of the zygomaticus when targeting the LLS may occur, resulting in a crooked smile. This can be corrected by chemodenervation of the contralateral zygomaticus.
Finally, elevation of the nasal tip occurs with injection of the depressor septi nasi, though depending on the patient this may be a desirable outcome. Regardless, this consequence must be predicted and discussed prior to treatment.
Video Demonstration:
Dimpled Chin: Mentalis
Problem & Desired Outcomes:
The mentalis is the prominent muscle on the chin, running vertically to connect the soft tissue of the chin inferiorly and the central mandible superiorly. Contraction results in upward traction on the lower free tissues of the mentum, bringing these soft tissues superiorly. In turn, there is an upward and outward motion of the lower lip. Given attachments to overlying cutaneous tissues, dimpling of the skin results. Hyperactivity at rest results in a pebbled appearance of the chin. Neurotoxin injection to the mentalis ameliorates this tense appearance (Figure 12). Of note, neurotoxin injection also represents a treatment for geniospasm, a rare hereditary trembling of the mentalis.12

Injection Sites & Surface Anatomy:
Localization of the mentalis is straightforward as the lower muscle belly is readily palpable when patients are asked to pout. As the lower portion is broader, inferiorly placed injections may be more predictable. Laterally positioned injection sites may inappropriately target the DLI, while injections near or above the mental crease may target either the orbicularis oris or the DLI, which overlies the mentalis at its superior portion. A useful rule of thumb is to keep injections superficial and at least 1cm below the mental crease (Figure 13). Either 1 or 2 injection sites per side may be performed dependent on an individual’s anatomy; 2 injections per side may prevent residual areas of dimpling.

Dose:
The required neurotoxin dose to this area is variable based on baseline activity of the mentalis, but the equivalent of 2-4U of onabotulinum per side is a representative starting range.
Potential Complications:
Overtreatment of the mentalis generally does not result in oral incontinence, as this muscle is only involved in compensatory mechanisms of oral competency. As with the orbicularis, symmetric injections of the mentalis are necessary to avoid a whorled appearance of the chin. Fortunately, this complication is easily corrected by additional injections of neurotoxin into the undertreated side. Perhaps most importantly, laterally or superiorly displaced injection sites may result in chemodenervation of the DLI. When this occurs, the lower lip curls over the lower teeth hiding this portion of the smile (Figure 14).

Video Demonstration:
Neck Bands & Nefertiti Face Lift: Platysma
Problem & Desired Outcomes:
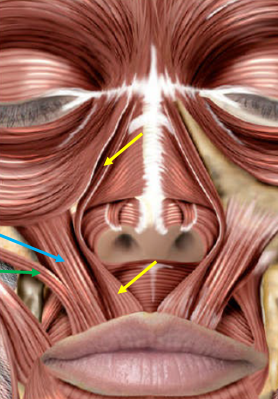
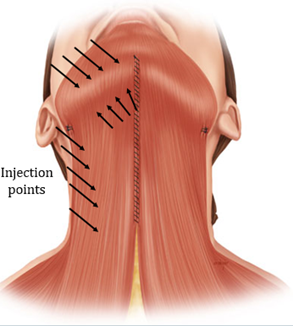
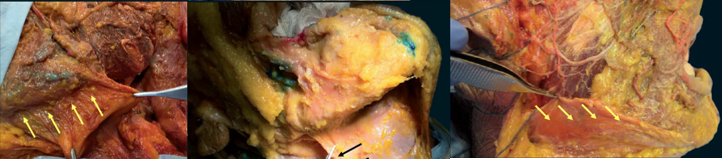
The platysma is a broad muscle that connects the thorax to the head. With abundant attachments at its superior terminus, including muscle fibers entwined with the DAO, DLI, and orbicularis oris as well as attachments at the mandible, modiolus, and lips, the platysmus is the most widespread downwardly-directed muscular force influencing the appearance of the lower face. Three components of the platysma – the pars mandibularis (attaching to the mandible), pars labialis (attaching to the lower lip), and pars modiolaris (attaching to the modiulus) – in part explain its underappreciated impact on the lower face.13 Contraction of the mandibular component of the platysma results in horizontal aggregations of skin inferior to the DAOs at the mid-mandible while contraction of the labial component results in similarly oriented horizontal lines inferior and lateral to the mouth.13 Contraction of the pars modiolaris results in vertically oriented creasing lateral to the mouth.13 These various effects are pictured in Figures 15-17. Altogether, its superior attachments complement the inferolateral pull of the DAOs on the oral commissures and of the depressor muscles on the lower lip.
At its inferior end, the platysma spans from shoulder to shoulder with anterior attachments near the clavicles. Contraction exacerbates wrinkling of the décolleté and the superior breasts.14 Finally, between the head and chest, the platysma runs superficially in the neck where, upon contraction, aggregation of its fibers can be seen as neck bands, which are easily identified and treated with neurotoxin, resulting in potentially broad positive impacts on rejuvenation of the lower face. In one study of platysmal chemodenervation, provider and patient satisfaction was 93.3% and 96.6%, respectively.15 In addition to minimizing perioral rhytids, improving the appearance of the décolleté, and concealing neck bands, treatment may result in a more defined jawline with less “jowling” (Figures 15-17). Younger patients or patients with notable elastic recoil of the neck skin are optimal candidates.



Injection Sites & Surface Anatomy:
Multiple injection sites are necessary to target the broad-ranging contractile functions of the platysma. Neck bands are the easiest to identify and treat, and can be accentuated by having the patient grimace, show their lower teeth, or say the letter “E.” Prior to injection, the neck bands should be pinched by the injector to ensure the muscle belly is appropriately targeted and that toxin is not accidentally placed too deep. Three to five injections oriented along the length of each neck band may be necessary, depending on the strength of contraction (Figure 18). The most posterior platysmal band is typically the strongest, while the number and strength of the anteriorly located bands is more variable.
Treatment of the superior portions of the platysma at the level of the mandible can be considered to more specifically ameliorate horizontal neck lines and vertical smile lines. Some advocate for a single line of 4 injections just beneath the edge of the mandible (1cm below), starting with the site of attachment of the posterior platysmal band and moving anteriorly.16 Injections along the mandible can be almost to bone. Other techniques include adding an additional parallel row of injection points just above the edge of the mandible (Figure 18 & 19).13
Dose:
Doses of neurotoxin necessary to achieve clinically meaningful inhibition of the platysma are the highest of any muscle in the head and neck; indeed, cadaveric studies have demonstrated that the mass of the platysma is five times that of the corrugators.3 Depending on the strength of contraction and the palpable muscle mass, a range of 15-50 U of onabotulinum or 40-125 U of abobotulinum or equivalent may be necessary for treatment. These doses vary significantly resulting from individual differences in muscle mass and strength, and it is crucial to adjust the doses accordingly. Younger men may require 50U while some older women may notice neck weakness after as few as 20-25 units. Doses should be distributed evenly based on the contributive contractile force of each neck band and region of the platysma. Given the higher doses of neurotoxin required, cost may be a significant deterrent to optimal treatment.
Potential Complications:
The most common symptom noted following treatment of neck bands is weakness in raising the head from a lying position, as might be encountered with exercise. This can be avoided by using less than 40 units of onabotulinum or equivalent per session, to avoid overwhelming weakness. Patients should be counseled on this possibility prior to injection, as many will experience a sensation of mild neck weakness.
Deep injections into the anterior neck bands can also be problematic. Dysphagia and vocal cord paralysis may occur should the toxin spread or be injected in the peripharyngeal muscles, which may occur if injections are placed below the level of the thyroid cartilage.3 Injections along the mandible can chemodenervate the submandibular gland, if placed too inferiorly, resulting in xerostomia (see below). Deep injections above the level of the mandible could inadvertently chemodenervate the mentalis, DLI, DAOs, or buccinators, which may require contralateral correction of symmetry.
Though not a complication per se, appropriate selection of candidates for treatment of platysmal bands is necessary. Patients with significant skin ptosis and redundant cutaneous neck tissues prior to the procedure may not have adequate elastic recoil to benefit from a neurotoxin-mediated necklift, and surgical approaches may be needed. Additionally, other platysmal bands may be recruited and compensate for those which have been chemodenervated, though this is typically to a lesser extent than originally was present and can easily be corrected with additional injections to the newly recruited bands.
Video Demonstration:
Jaw Shaping, Bruxism: Masseter
Problem & Desired Outcomes:
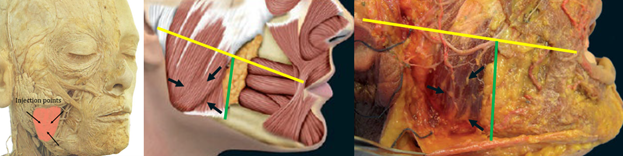
The masseter is a muscle of mastication that can be targeted via neurotoxin for functional and aesthetic purposes. Although there are attachments via aponeuroses to the coronoid process and zygomatic arch superiorly, the thickest portion of the masseter is located closer to the angle of the mandible.3 Contraction acts to appose the posterior mandibular dentition to the maxillary molars. With time, an overactive masseter can hypertrophy, resulting in a squared lower face. This may be particularly prevalent in patients of Asian descent. Unlike dynamic rhytids, masseter hypertrophy is most common between 20 and 40 years of age, since the teeth may deteriorate thereafter and prevent successful masseter driven apposition.17 Notably, age related bone-resorption of the maxilla and mandible may be caused in part by jaw clenching, highlighting the potential value of this treatment in severely afflicted subjects.18 Chemodenervation of the masseter can induce atrophy, decreasing its size by 20-30%. The result is a more slender and potentially more feminine jawline (Figure 20). Notably, the masseter may also be treated to improve symptomatic temporomandibular joint dysfunction, bruxism, or malocclusion resulting from asymmetric strength.

Injection Sites & Surface Anatomy:
The masseter is easily palpated upon jaw clenching. Precise injections are necessary to avoid the facial artery and vein anteriorly, the risorius superiorly, and the parotid posteriorly. Cadaveric studies have shown that the lower portion of the masseter has the densest innervation, confirming the appropriateness of this area for neurotoxin injection.19 There are several techniques for injection, but in general three injection sites in a triangular orientation are commonly performed.3,20 The precise localization of injection points is individualized on the basis of palpation. The first injection site is typically into the thickest palpable portion of the masseter. This tends to be the most anterior and superior injection site. This injection point should be 1cm from the anterior border of the masseter. It should remain below an imaginary line drawn from the tragus to the oral commissure. The other two injection points are placed 1.5-2cm apart along an imaginary line 5mm above and parallel to the mandible (Figure 21). Deep injections into the muscle belly are necessary.3,20
Dose:
Effective doses for treatment of the masseter range from 20 to 40 units of onabotulinum toxin or equivalent.20 Doses of 10-20U of onabotulinum may be inadequate.21 One study found that 25-30 units of onabotulinum toxin was sufficient in Caucasian patients, while 40 units were necessary in Asian patients to achieve a similar result.22 Higher doses over a shorter period may result in a more rapid reduction, while lower doses over greater time can induce a more gradual atrophy.23 Injections are distributed evenly among the 3 injection points.
Potential Complications:
Several complications are possible with injection of the masseter. Discomfort at the injection site is the most common adverse reaction, though it does not generally impact quality of life.20,24 If injections are anteriorly and superiorly displaced from the target site, they may target the risorius or levator anguli oris muscles resulting in a crooked smile. From a vascular perspective, anterior injections may also target the facial artery or vein, resulting in pain, swelling, or ecchymosis. Therefore, injections are not recommended within 1cm or less of the anterior border of the masseter.
On the other hand, injections too far posteriorly and not into the muscle may affect the parotid. The parotid has been demonstrated to overlie the majority of the masseter in a proportion of patients, though the anterior portion of the muscle appears spared.25 Bilateral injections of the parotids or parotid duct may result in xerostomia (see below).
Failure to note asymmetries pre-injection or injection of uneven doses of neurotoxin can theoretically create or potentially malocclusion; interestingly however, unilateral injections have been shown to potentially impact both masseters, making this complication less likely to occur in practice.20 Failure to treat the deep portions of the masseter can result in an outward protrusion of the masseter that appears as a bulge. This can be corrected by injection of 5-10U of onabotulinum or equivalent at the bulging area.20,24
In older patients, tissue laxity following masseter atrophy may be problematic (Figure 22). This complication may possibly avoided by using conservative dosing (10-15U of Onabotulinum per side) in women over 40 years of age. Chemodenervation of the overlying platysma may be a partial remedy as well. Given superior attachments to the zygomatic arch and coronoid process, excessive hollowing of the infrazygomatic region may also occur when the masseter is relaxed. Filler injection may be considered in the latter, though selection of appropriate candidates for masseter treatment is key; fortunately, the demographic affected most by hypertrophy tends to be younger.

Video Demonstration:
Facial Shaping: Parotid, Submandibular Glands
Problem & Desired Outcomes:
The cholinergic innervation of the salivary glands makes them susceptible to treatment with botulinum toxins. Functionally, this can be used to treat sialorrhea. With chemodenervation, the salivary glands decrease in size and therefore this technique can be harnessed for facial shaping in select candidates. Treating the parotid glands can cause slimming of the face and improved definition of the jawline from above the mandible. It is important to separate hypertrophy of the masseters from hypertrophy of the parotids, as the former problem must be addressed separately (see above). The body of the parotid is located posterior to the mandible, though the two tissues may overlap significantly.
Prominence of the submandibular glands is common with aging and may be especially noticeable following facial rhytidectomy. Shrinkage of the submandibular glands can improve the contour of the upper neck, decrease the appearance of the jowls, and improve jawline definition from below the level of the mandible. This can complement treatment of jowling via chemodenervation of the platysma or deoxycholic acid injections. Optimal results of parotid and submandibular gland injections are pictured in Figure 23 & Figure 24, respectively.

Injection Sites & Surface Anatomy:
The inconspicuous positioning of the parotid and submandibular glands can make precise localization of injection points difficult. Localization of the salivary glands via careful palpation in the area posterior to the masseter for the parotid and in the jowls for the submandibular can direct the injector to the most appropriate injection site, though this is often subtle. For treatment of sialorrhea, many recommend the use of ultrasound guided injections to ensure the glands – and not surrounding structures – are targeted.26 For aesthetic indications however, injections are typically performed only if the glands are externally visible, thus obviating the need for ultrasound.
Dose:
For the parotids, a dose of up to 40 U onabotulinum per side each month for 3-4 months until reduction is reached can be considered.23 Doses may be divided to target the most several most significantly enlarged areas of the parotid. 20 U of onabotulinum per submandibular gland may be a starting dose. Reported doses are highly variable, from as little as 10 U to the submandibular glands to 100 U per side to the parotid.26 The lowest dose possible is recommended to avoid complications, and higher concentrations of toxin can be considered to limit spread to the strap and peripharyngeal muscles of the neck. Maintenance injections at least every 6 months may be necessary after the desired endpoint is reached.23
Potential Complications:
Xerostomia can result from overaggressive treatment of the parotid and submandibular glands, though this appears to be an uncommon complication.23 Even with ultrasound guidance, several adverse effects in children treated for sialorrhea have been reported, including aspiration pneumonia, severe dysphagia, and loss of motor control of the head, though many of these patients had underlying neurodevelopmental conditions (e.g. cerebral palsy).27 Nevertheless, the potential for salivary gland neurotoxin injection to result in speech or swallowing difficulty must be considered given the proximity of the mylohyoid, platysma, and digastric muscle to the submandibular gland. Of note, one small study found no changes in cariogenic bacteria following injections for sialorrhea.28
Video Demonstration:
Conclusion
Meticulous technique and careful patient selection can result in reproducible and aesthetically pleasing rejuvenation using neurotoxin for treatment of the lower face. Injectors should have a firm grasp of the anatomy of target structures and a strong understanding of potential complications resulting from inaccurate injection or inappropriate candidate selection.
Notably, aesthetic treatment of the lower face is not limited to neurotoxin injection; rather, neuromodulator use in combination with filler injections, light-based treatments, topical therapies, or surgical approaches may be necessary depending upon a patient’s unique facial structure, skin quality, and desired outcome. This is supported by evidence such as the fact that neurotoxin injections increase the efficacy of, and patient satisfaction with, hyaluronic acid fillers.29,30 Additionally, many strategies used to treat the upper face, such as hyaluronic acid filler injections to the temporal fossae or zygomatic region, may secondarily improve the appearance of the lower face by providing upward lift to these areas. An integrated approach to rejuvenation is therefore necessary to achieve an optimal result.
References
- Shaw RB, Jr., Katzel EB, Koltz PF, et al: Aging of the facial skeleton: aesthetic implications and rejuvenation strategies. Plast Reconstr Surg 127:374-83, 2011
- Richard MJ, Morris C, Deen BF, et al: Analysis of the Anatomic Changes of the Aging Facial Skeleton Using Computer-Assisted Tomography. Ophthalmic Plastic & Reconstructive Surgery 25:382-386, 2009
- Trevidic P, Sykes J, Criollo-Lamilla G: Anatomy of the Lower Face and Botulinum Toxin Injections. Plast Reconstr Surg 136:84S-91S, 2015
- Kane MA: The functional anatomy of the lower face as it applies to rejuvenation via chemodenervation. Facial Plast Surg 21:55-64, 2005
- Wu DC, Fabi SG, Goldman MP: Neurotoxins: Current Concepts in Cosmetic Use on the Face and Neck–Lower Face. Plast Reconstr Surg 136:76S-79S, 2015
- Cohn JE, Greco TM: Advanced Techniques for the Use of Neurotoxins in Non-Surgical Facial Rejuvenation. Aesthetic Plast Surg, 2020
- Benedetto A: Botulinum Toxins in Clinical Aesthetic Practice, Taylor & Francis Ltd, 2011
- Kim NH, Ahn TJ, Park RH, et al: A Simplified Approach to Botulinum Toxin Injection for the Lower Face: Concept of a 24-Hour Clock. Plast Reconstr Surg 139:816e-818e, 2017
- Sucupira E, Abramovitz A: A simplified method for smile enhancement: botulinum toxin injection for gummy smile. Plast Reconstr Surg 130:726-8, 2012
- Mazzuco R, Hexsel D: Gummy smile and botulinum toxin: a new approach based on the gingival exposure area. J Am Acad Dermatol 63:1042-51, 2010
- Hwang WS, Hur MS, Hu KS, et al: Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin. Angle Orthod 79:70-7, 2009
- Gonzalez-Alegre P, Kelkar P, Rodnitzky RL: Isolated high-frequency jaw tremor relieved by botulinum toxin injections. Mov Disord 21:1049-50, 2006
- de Almeida ART, Romiti A, Carruthers JDA: The Facial Platysma and Its Underappreciated Role in Lower Face Dynamics and Contour. Dermatol Surg 43:1042-1049, 2017
- Benedetto AV: What’s New in Cosmetic Dermatology. Dermatol Clin 37:117-128, 2019
- Jabbour SF, Kechichian EG, Awaida CJ, et al: Botulinum Toxin for Neck Rejuvenation: Assessing Efficacy and Redefining Patient Selection. Plast Reconstr Surg 140:9e-17e, 2017
- Levy PM: Neurotoxins: Current Concepts in Cosmetic Use on the Face and Neck–Jawline Contouring/Platysma Bands/Necklace Lines. Plast Reconstr Surg 136:80S-83S, 2015
- Franks AS: Masticatory muscle hyperactivity and temporomandibular joint dysfunction. J Prosthet Dent 15:1122-31, 1965
- Bartlett SP, Grossman R, Whitaker LA: Age-related changes of the craniofacial skeleton: an anthropometric and histologic analysis. Plast Reconstr Surg 90:592-600, 1992
- Kim DH, Hong HS, Won SY, et al: Intramuscular nerve distribution of the masseter muscle as a basis for botulinum toxin injection. J Craniofac Surg 21:588-91, 2010
- Almukhtar RM, Fabi SG: The Masseter Muscle and Its Role in Facial Contouring, Aging, and Quality of Life: A Literature Review. Plast Reconstr Surg 143:39e-48e, 2019
- Choe SW, Cho WI, Lee CK, et al: Effects of botulinum toxin type A on contouring of the lower face. Dermatol Surg 31:502-7; discussion 507-8, 2005
- Liew S, Dart A: Nonsurgical reshaping of the lower face. Aesthet Surg J 28:251-7, 2008
- Wu WT: Botox facial slimming/facial sculpting: the role of botulinum toxin-A in the treatment of hypertrophic masseteric muscle and parotid enlargement to narrow the lower facial width. Facial Plast Surg Clin North Am 18:133-40, 2010
- Park MY, Ahn KY, Jung DS: Botulinum toxin type A treatment for contouring of the lower face. Dermatol Surg 29:477-83; discussion 483, 2003
- Hu KS, Kim ST, Hur MS, et al: Topography of the masseter muscle in relation to treatment with botulinum toxin type A. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110:167-71, 2010
- Bae GY, Yune YM, Seo K, et al: Botulinum toxin injection for salivary gland enlargement evaluated using computed tomographic volumetry. Dermatol Surg 39:1404-7, 2013
- Chan KH, Liang C, Wilson P, et al: Long-term safety and efficacy data on botulinum toxin type A: an injection for sialorrhea. JAMA Otolaryngol Head Neck Surg 139:134-8, 2013
- Tiigimae-Saar J, Taba P, Tamme T: Does Botulinum neurotoxin type A treatment for sialorrhea change oral health? Clin Oral Investig 21:795-800, 2017
- Carruthers A, Carruthers J, Monheit GD, et al: Multicenter, randomized, parallel-group study of the safety and effectiveness of onabotulinumtoxinA and hyaluronic acid dermal fillers (24-mg/ml smooth, cohesive gel) alone and in combination for lower facial rejuvenation. Dermatol Surg 36 Suppl 4:2121-34, 2010
- Carruthers J, Carruthers A, Monheit GD, et al: Multicenter, randomized, parallel-group study of onabotulinumtoxinA and hyaluronic acid dermal fillers (24-mg/ml smooth, cohesive gel) alone and in combination for lower facial rejuvenation: satisfaction and patient-reported outcomes. Dermatol Surg 36 Suppl 4:2135-45, 2010

