Introduction
As the dorsum of the hand is visible during most activities of daily life, patients often seek plastic surgeons with the goal of restoring smooth, youthful, aesthetic appearing hands. This attention to the aesthetic appearance of youthful hands has led to the evolution of techniques for hand rejuvenation. Aging hands are a normal part of aging, usually paralleling aging of the face and other parts of the body, and characterized by wrinkles, hallowing of the dorsal web spaces, and prominence of extensor tendons and veins[1-3]. Dr. Pierre F. Fournier first described the use of autologous fat for hand rejuvenation in 1988. Over the years, his technique was refined however as injectable dermal fillers ( hyaluronic acid and calcium hydroxylapatite) became available they began being used off label, with excellent results and have gained favor over fat grafting. A calcium hydroxylapatite filler was FDA-approved in 2015 as the first injectable filler for hand augmentation to correct volume loss[4]. Many techniques for hand rejuvenation have been described, including the use of fat[3-6], fillers [3, 4, 7, 8], skin excision[3, 9], resurfacing[3, 10], sclerotherapy[3, 11], and a combination approach [3, 12, 13]. Herein, we describe the use of fat grafting, and injectables in their role for hand rejuvenation and volume restoration.
Fat
Fat grafting has been used for years and has proven to be effective in reshaping and rejuvenating aging hands. In fact, the first injection-based technique for hand rejuvenation was an autologous fat graft, described by Pierre F. Fournier in 1988. Since then, fat grafting has remained a desirable technique for hand rejuvenation largely because it is an autologous source that is readily available and relatively easy to harvest. Autologous fat allows for the treatment of volume and contour defects. Prominent veins, and extensor tendons can be masked, providing smooth and youthful contour. Studies have demonstrated that the addition of adipose may also play a role in rejuvenation of the deep and superficial skin tissue [6].
However, fat grafting does not come without disadvantageous as fat grafting is associated with donor site morbidity, commonly contour irregularities from donor site harvest, along with an increased risk of infection to the donor site. The flank, periumbilical region, and thigh are the donor sites most commonly used[6]. Rohrich et al. did not find any significant difference in cell viability in adipose tissue removed from the different donor sites[14]. Although fat harvest under local anesthesia has been described and is used, we prefer the use of MAC anesthesia in the operating room setting for the safety and comfort of our patients.
Fat Grafting Surgical Technique:
Fat grafting of the hands is a relatively simple procedure; however we prefer to perform fat harvest in the operating room setting under MAC and local anesthesia. Many studies have looked at the effects of prior infiltration/local anesthesia before fat harvest. Moore et al. concluded no significant effect on cell attachment in culture, morphology, proliferation or adipose metabolic activity [15]. These studies suggest the use of epinephrine, or local anesthesia should be used for pain relief, or hemostatic control rather than cell viability[16].
Fat extraction is used using a 3.0mm outer diameter cannula. We recommend collecting between 30-50 cm3 of fat, and decanting for 10 minutes. Approximately 5cc of local anesthetic is then injected along the dorsum of the hand and 15-25cm3 of fat is injected using a 1.4mm outer diameter cannula into the dorsum of the hand, from the wrist. Careful attention must be given to gently inject into the dorsal deep fascia, and to not inject fat into the veins, or dorsal extensor tendons of the hand. The fat is gently massaged into place. We recommend prophylaxis antibiotics with cephalexin. Patients should return to clinic for check ups at 24 hours, 7 days, 1 month, and 6 months for posttreatment evaluation.
Calcium Hydroxylapatite Fillers
Although patients have been seeking treatment to restore aging hands for years, the first injectable filler for the hand was only recently approved by the Food and Drug Administration in 2015. CaHA fillers contain 70% CaHA microparticles in 70% aqueous carboxymethylcellulose gel carrier[4]. These large particles provide durability as they are not effectively broken down by macrophages, stimulating fibroblast ingrowth and collagen formation around the microspheres[4]. Therefore, CaHA not only provides hand rejuvenation, but may also improve skin quality through collagen stimulation. The firmness of the product along with its reduced solubility may also lead to a “clumpy” feel or appearance. It has been reported to last up to 2 years after administration.
Hyaluronic Acid Fillers
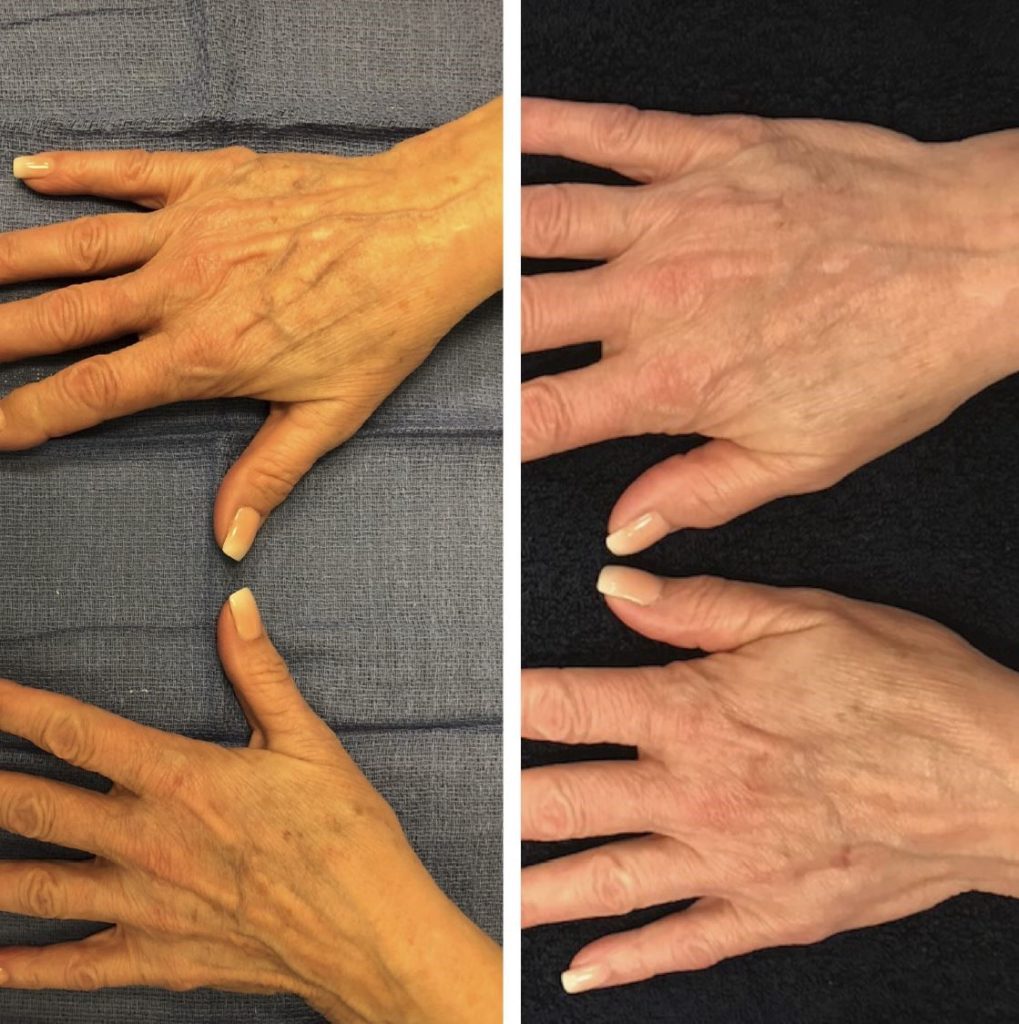
HA is a glycosaminoglycan biopolymer composed of strands of repeating chains of d-glucuronic acid and H-acetyl-d-glucosamine[17]. The first HA dermal filler became available in 2003. Over the years, it gained increasing popularity for its ease of use, and excellent results and was becoming used off label for hand rejuvenation. HA fillers quickly gained popularity over fat grafting due to the lack of donor site morbidity, ease of use, and more consistent results. HA restores volume, thereby improving skin elasticity and reducing the appearance of wrinkles, prominent veins and tendons of the aging hands. When administered by a trained and experienced clinician, it provides fantastic results lasting up to 6 months with minimal adverse effects. For these reasons, and its ease of use in an outpatient setting, we prefer the use of HA in our practice.
CaHA and HA Fillers Technique
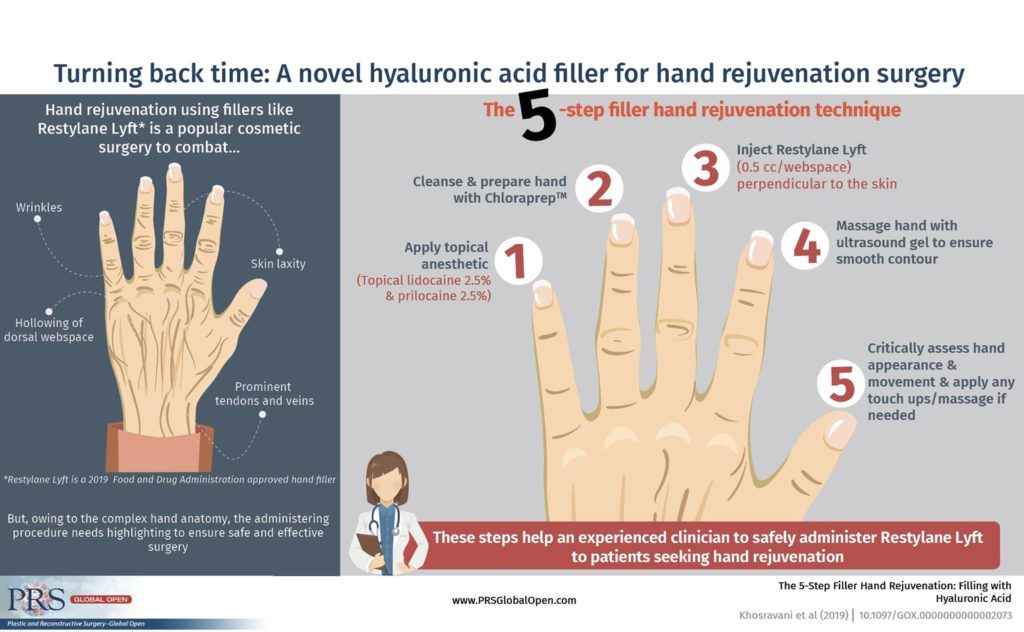
The authors of this paper previously published “The 5-Step Filler Hand Rejuvenation: Filling with Hyaluronic Acid” [1], which demonstrates the technique for safely and effectively applying hand fillers. It is absolutely critical for the plastic surgeon or clinician to understand the mechanism of aging and have expertise with the anatomy of the dorsum of the hand, as careless application can lead to injury to the dorsal veins, extensor tendons, and sensory nerves with potentially lasting consequences. Bidic et al. described the anatomy of the hand in distinct layers starting from superficial: skin, dorsal superficial lamina, dorsal superficial fascia, dorsal intermediate lamina, dorsal intermediate fascia, dorsal deep lamina and dorsal deep fascia[3]. The desired plane for injection is the dorsal superficial lamina, which is the fatty layer deep to the skin, lacking sensory nerves and major veins. However, it contains various longitudinally running septa thereby requiring gentle massage for even distribution along each webspace.
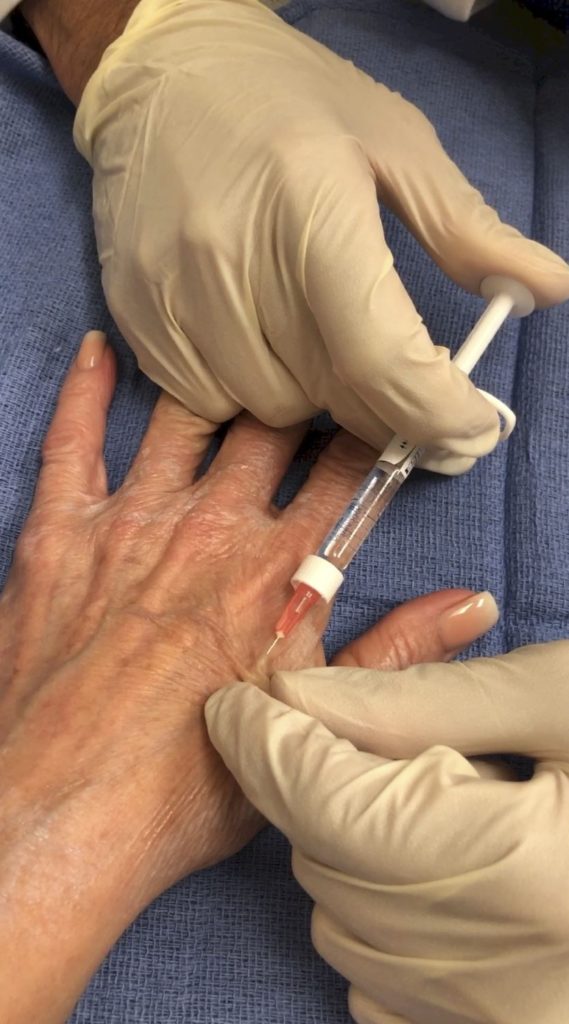
Our 5-step technique begins with application of topical lidocaine and prilocaine to the dorsal aspect of the hands. (Figure 1.) After 20 minutes, both hands are then prepped with Chloraprep TM to cleanse the hands. (Figure 2.) Next, the four dorsal web spaces are injected with small aliquots of dermal filler, approximately 0.5cc/webspace. The injection is performed by tenting the skin and injecting the filler perpendicular to the skin taking great care to avoid the dorsal veins and extensor tendons. This is facilitated by ensuring the injections are in the dorsal superficial and dorsal intermediate layer avoiding the dorsal deep layer. (Figure 3.) The aliquots are massaged around the webspace using ultrasound gel and the hands are reevaluated to circumvent overfilling of the material causing contour irregularity. (Figure 4.) Finally, both hands are assessed critically to ensure appropriate rejuvenation and youthful harmony without compromise of hand function. (Figure 5.) Any touch ups or with filler can be performed at this time followed by massaging with the gel. The patient then should return to clinic in 1 week, 1 month and 6 months for post treatment evaluation. (Figure 6)




Discussion
Aging hands are a normal part of the aging process characterized by wrinkles, hollowing of the dorsal webspace’s, and prominence of veins and extensor tendons. As patients seek rejuvenation with the goal of restoring youthful appearing hands, clinicians must be well versed in the various techniques for hand rejuvenation to be able to provide the patient with a realistic satisfying outcome. While fat grafting has the benefits of having an autologeous source that is readily available, donor site morbidity and the need for the operating room for fat harvest make it less desirable. The authors of this paper prefer the use of injectables for hand rejuvenation, specifically with HA due to its solubility, ease of use, fantastic and consistent results. However, both when used by experienced clinicians will prove effective in enhancing youthful appearing hands.
However, despite the seemingly ubiquitous use of fillers, patients must seek experienced clinicians, with strong understanding of hand anatomy. Complications can be lasting and devasting. An understanding of the dorsal layers of the hand as well as proper technique is crucial to prevent injection into vessels, nerves, and tendons.
- Khosravani, N., et al., The 5-Step Filler Hand Rejuvenation: Filling with Hyaluronic Acid. Plast Reconstr Surg Glob Open, 2019. 7(1): p. e2073.
- Jakubietz, R.G., et al., The ageing hand. A study to evaluate the chronological ageing process of the hand. J Plast Reconstr Aesthet Surg, 2008. 61(6): p. 681-6.
- Bidic, S.M., D.A. Hatef, and R.J. Rohrich, Dorsal hand anatomy relevant to volumetric rejuvenation. Plast Reconstr Surg, 2010. 126(1): p. 163-8.
- Rivkin, A.Z., Volume correction in the aging hand: role of dermal fillers. Clin Cosmet Investig Dermatol, 2016. 9: p. 225-32.
- Giunta, R.E., et al., [Structural fat grafting for rejuvenation of the dorsum of the hand]. Handchir Mikrochir Plast Chir, 2010. 42(2): p. 143-7.
- Fantozzi, F., Hand rejuvenation with fat grafting: A 12-year single-surgeon experience. Eur J Plast Surg, 2017. 40(5): p. 457-464.
- Vleggaar, D., Soft-tissue augmentation and the role of poly-L-lactic acid. Plast Reconstr Surg, 2006. 118(3 Suppl): p. 46s-54s.
- Graivier, M.H., et al., Calcium Hydroxyapatite (CaHA) Indication for Hand Rejuvenation. Aesthet Surg J, 2018. 38(suppl_1): p. S24-s28.
- Wendt, J.R., Distal, dorsal superior extremity plasty. Plast Reconstr Surg, 2000. 106(1): p. 210-3.
- Weiss, D.D. and J.H. Carraway, Hand rejuvenation. Aesthet Surg J, 2004. 24(6): p. 567-73.
- Lee, B.J., The role of sclerotherapy in abnormal varicose hand veins. Plast Reconstr Surg, 2000. 106(1): p. 227-9.
- Butterwick, K. and N. Sadick, Hand Rejuvenation Using a Combination Approach. Dermatol Surg, 2016. 42 Suppl 2: p. S108-18.
- Shamban, A.T., Combination hand rejuvenation procedures. Aesthet Surg J, 2009. 29(5): p. 409-13.
- Rohrich, R.J., E.S. Sorokin, and S.A. Brown, In search of improved fat transfer viability: a quantitative analysis of the role of centrifugation and harvest site. Plast Reconstr Surg, 2004. 113(1): p. 391-5; discussion 396-7.
- Moore, J.H., Jr., et al., Viability of fat obtained by syringe suction lipectomy: effects of local anesthesia with lidocaine. Aesthetic Plast Surg, 1995. 19(4): p. 335-9.
- Gir, P., et al., Fat grafting: evidence-based review on autologous fat harvesting, processing, reinjection, and storage. Plast Reconstr Surg, 2012. 130(1): p. 249-58.
- Tezel, A. and G.H. Fredrickson, The science of hyaluronic acid dermal fillers. J Cosmet Laser Ther, 2008. 10(1): p. 35-42.
