Abstract
Complementing popular rejuvenation modalities for the face, cosmetic treatments for other areas of the body are in high demand among patients who want to achieve a more global youthful appearance. Arm rejuvenation is just one of many exciting and obvious new landscapes to this effect. In recent years and with the emergence of more revolutionary treatment options, the paradigm of a single modality approach has fallen largely out of favor in rejuvenation of the face, neck and chest. Similarly, optimizing cosmetic outcomes in arm rejuvenation nearly always requires multimodal combination therapy. With an ever-expanding armamentarium of treatment options that range from fillers, laser and light-based devices, radiofrequency and ultrasound, total arm rejuvenation is an attainable outcome with high rates of patient satisfaction.
Introduction
Complementing popular rejuvenation modalities for the face, cosmetic treatments for other areas of the body are in high demand among patients who want to achieve a more global youthful appearance. Arm rejuvenation is just one of many exciting and obvious new landscapes to this effect. In recent years and with the emergence of more revolutionary treatment options, the paradigm of a single modality approach has fallen largely out of favor in rejuvenation of the face, neck and chest. Similarly, optimizing cosmetic outcomes in arm rejuvenation nearly always requires multimodal combination therapy. With an ever-expanding armamentarium of treatment options that range from fillers, laser and light-based devices, fat reduction methods, radiofrequency and ultrasound, total arm rejuvenation is an attainable outcome with high rates of patient satisfaction.
Arm rejuvenation
Anatomy
With its unique anatomy and highly specialized functions, the arms age in ways that pose unique challenges relative to other areas of the body. Just as structural changes to bone, musculature and subcutaneous tissues of the face contribute largely to the characteristics associated with aging, a similarly intimate relationship between skin, muscle and bone explains the ways the arms age over time. Analogous to the osteopenia in which age-related resorption of bone in the zygoma and mandible lead to the undesirable appearance of deep nasolabial folds and jowls, respectively, resorption of bone in response to hormonal factors, osteoporosis and remodeling from injury also occurs in the bones of the arms. As the internal structures of the arms thin from osteopenia, the soft tissue and skin appear hyperlinear and lax.
This laxity is further exacerbated by atrophy of muscles, or sarcopenia, such as the pectoralis major, latissimus dorsi, deltoid, and those of the rotator cuff that move the upper arm; and the muscles of the anterior and posterior component of the arm and forearm including the triceps brachii, biceps brachii, brachialis, and brachioradialis. Taken together, these structural changes to bone and muscle result in profound loss of volume and, consequently, decreased support for overlying tissue.
At the cutaneous level, too, the arms are subject to similar age- and UV-related microstructural changes as the face. Progressively waning amounts of collagen, elastin and other glycosoaminoglycans, such as hyaluronic acid, further exacerbate skin laxity and the crepey texture most patients find cosmetically undesirable. The repetitive torque and twisting motions of the arm create areas of extra hyperlinear rhytids above and below the antecubital fossa and the anterior axillary fold at the insertion points of the pectoralis major muscle in the humerus. Dyspigmentation from solar lentigines and poikiloderma, as well as age related asteatosis, and small keratoses, both actinic and seborrheic, all contribute to patient dissatisfaction.
Anatomic considerations when treating the arms include neurovascular structures, tendons, and ligaments as they pertain to the three joints of the shoulder, elbow, and wrist. General knowledge of the pathways and depth of the neurovasculature is expected before performing cosmetic treatments of the arm. In particular, special caution must be taken in the danger zones of the axillae, antecubital fossa, and epicondyle, where critical nerves run superficially and are at risk for neuropraxia. These nerves originate from C5-T1 and merge forming the brachial plexus that divides into the musculocutaneous, axillary brachial, radial, and ulnar nerves.
The brachial artery of the arm splits at the cubital fossa into the brachial and ulnar arteries and their tributaries. Venous drainage consists of the basilic, cephalic and median forearm veins, which tribute to the two brachial veins which drain into the axillary and finally subclavian veins. Given the larger caliber and collaterality of this vasculature compared with the facial vessels, occlusion and ischemia are a less obvious concern. When they occur, however, hematomas develop rapidly in the arms, which may lead to acute and chronic inflammation and a higher risk of infection. Infection is uncommon, but obtaining the patient’s history, as for lymphedema and prior surgery, is essential for the arms, as is the need to follow the same aseptic cleaning protocols as for the face and hands. Though these complications are overall rare, since larger volumes of fillers may be injected in the compartments of the arm to achieve optimal results, it is still necessary to be cognizant of these risks. The lower complication risk when treating the arms is attributable, at least in part, to the relatively abundant adipose tissue that protects the underlying ligaments, tendons, muscles, and deeper neurovascular structures.
Treatment Options
To ensure holistic rejuvenation of the arms, several cosmetic concerns must be addressed. To do so usually requires variable combinations of a superficial tightening device, deeper tightening device, visible light technology to address dyschromia, dilute or hyper-dilute dermal fillers, and a method to address excess adiposity. Chemical peels, microdermabrasion and dermabrasion can also be used for arm rejuvenation, however, they will not be discussed herein owing to our belief that they are overall less successful at producing significant improvements. It is important to consider that, compared to facial skin, the skin on the arms is more difficult to rejuvenate with energy sources, owing to a thinner dermis with fewer adnexal structures, which portends poorer wound healing. Despite this, however, arm rejuvenation is possible and can be done with excellent outcomes using both energy and non-energy dependent sources.
Restorative techniques most commonly implemented in arm rejuvenation can be thought of as belonging to one of five groups – (1) modalities that broadly ablate and/or heat a very superficial layer of skin in a controlled fashion, (2) fractional non-ablative and ablative technologies, (3) technologies that directly target dyschromia, flushing, and telangiectasias,(4) skin-tightening technologies, such as radiofrequency and ultrasound, and (5) treatments that target excess adiposity, such as cryolipolysis and liposuction.
Dyspigmentation
The choice of treatment modality used to target dyspigmentation is dependent, in part, on the pattern in which the dyspigmentation presents. On the arms, dyspigmentation typically manifests in one of two ways. The first is as mottled hyper- and hypopigmentation (Figures 4 & 5), which may be seen in the presence of scattered and sometimes dense telangiectatic vessels (poikiloderma). The second is as discrete solar lentigines. In general, mottled pigmentation is optimally treated with laser and light-based modalities that distribute energy equally across a larger surface area, whereas discrete solar lentigines are better treated with pigment-specific lasers. However, the sheer size of the arm and the number of lesions the patient would like to treat over its surface area are factors to consider that sometimes require a deviation from this general strategy.
If one were to treat diffuse mottled pigmentation with small-diameter spot size–specific pigment lasers, cosmetically undesirable speckling may result. Consequently, devices capable of uniformly treating large surface areas are more appropriate. Among them, we prefer one of three modalities: the fractionated non-ablative 1,927-nm thulium fiber laser (Fraxel Dual; Solta Medical, Hayward, CA), the fractionated ablative 2,940-nm erbium:YAG (HALO, Sciton Inc., Palo Alto, CA) and broad band light (HERO, Sciton Inc). Intense Pulsed Light (IPL) is the same as BBL, however, the HERO technology is specifically for the safe and rapid treatment of larger surface areas at lower joules with a faster pulse delivery and a gliding handpiece rather than a spot by spot technique. Although originally all three were designed to treat dyspigmentation of the face, neck and chest, these technologies produce impressive results when used on the arms.
While an argument can be made for the use of either BBL or a fractionated 1,927-nm thulium fiber laser in the treatment of diffuse dyspigmentation, the former should always be the preferred modality in treating poikiloderma, owing to its ability to non-selectively target vascular as well as pigmented lesions. Simply stated, rather than using a single, focused wavelength of laser light, BBL and IPL use multiple light wavelengths filtered to within a narrow range such as 515nm. While both the fractional 1927nm and the BBL/IPL have the ability to promote collagen synthesis, BBL may be superior for discolorations by offering additional rejuvenation effects via improvements in erythema and pigmentation and texture. This is supported by a 2013 study published in the Journal of Investigative Dermatology, which found that BBL treatments restored gene expression patterns of photoaged and intrinsically aged human skin to more closely resemble young skin (Chang). Treatments with High Energy Rapid Output BBL (HERO; Sciton Inc., Palo Alto, CA) are particularly effective at treating the large surface area of an extremity, owing to energy delivery at faster rates than its predecessors.
The 1,927-nm thulium fiber laser is a non-ablative fractionated laser that is also highly effective at treating dyspigmentation, albeit by a different mechanism of action than that of BBL/IPL. This and the fractionated ablative 2,940-nm erbium:YAG laser function on the basis of fractionated photothermolysis (FP). FP is one of the greatest advancements in laser surgery owing, in part, to its ability to safely treat dyschromia, fine lines, and mild laxity on non-facial skin. This is particularly true of ablative lasers which, when employed on non-facial areas such as the extremities in an unfractionated form, carry a significant risk of potentially permanent scarring and hyperpigmentation.
An advantage of both the fractionated ablative 1,927-nm thulium fiber laser and the fractionated ablative 2,940-nm erbium:YAG laser is that they are incorporated into “dual” mode devices. Considering that the majority of patients looking to treat dyspigmentation on the arms also have skin laxity, a “dual” mode laser, which employs two different wavelengths, can be especially effective. By targeting multiple signs of aging, these dual wavelength lasers can offer more comprehensive rejuvenation. The 1,550-nm/1,927-nm dual wavelength laser (Fraxel:Dual, Solta Medical, Hayward, CA) incorporates a 1,550-nm fractionated non-ablative erbium:YAG laser for penetration into the deep dermis, where it stimulates neocollagenesis and neoelastinogenesis. When using the “dual” mode, some recommend first treating with the 1,550-nm at roughly 30 mJ and 15% density, followed by the fractionated 1927-nm laser at pulse energies of 5 to 10 mJ and surface densities ranging from 20% to 30%. Test spots are always important before full treatments should any concerns exist around optimal healing.
The dual 1,470 nm/2,940 nm laser (HALO, Sciton Inc., Palo Alto, CA) offers similar results in treating dyspigmentation on the arms as the 1,550-nm/1,927-nm dual wavelength laser. This is not surprising, considering that they are similar in many ways, with the non-ablative wavelengths (1,550-nm and 1,470-nm) being comparably more alike than the more superficial penetrating wavelengths. Much like the 1,550-nm erbium:YAG laser, the more deeply penetrating 1,470-nm non-ablative diode laser addresses fine lines and surface irregularities. The more superficial, ablative 2,940-nm erbium:YAG laser addresses superficial pigment. Typically, on non-facial areas such as the arms, total surface density coverage should not exceed 30% to 35%. Waibel and colleagues are more conservative and specifically recommend cross sectional area percentages less than 20% for both the 1,470-nm and 2,940-nm components when treating the body. Very recently, another dual fractional laser, the Clear + Brilliant Touch (Solta Medical, Inc., Bothell, WA) was upgraded to allow for rapid toggling from one wavelength to the next with lower mJ and less density, thus allowing for more rapid recovery. Ultimately, whether IPL or a fractionated dual wavelength laser is selected, it is important to remember that, because of variations in the skin of the arm, lower fluences and broader pulse durations (for IPL) or lower fluences and densities (for fractionated thulium fiber) compared to those used on the face are recommended so as to avoid excessive epidermal damage.
For those patients with discrete pigmented lesions on the arms, a more specific pigment-targeting laser is often more favorable. Particularly useful are quality-switched (Q-switched) and picosecond lasers, which are ideally suited for the treatment of solar lentigines because their short pulse durations allow for safe breakdown of small endogenous pigment chromophores with short thermal relaxation times. They have also been shown to induce neocollagenesis and neoelastinogenesis by way of generating laser-induced optical breakdown products at targeted cutaneous depths. Consequently, nano-and pico-second lasers provide partial restoration of skin structure and function, independent of their ability to treat pigmented lesions, making them an advantageous modality when approaching total arum rejuvenation.
Developed roughly two decades ago, Q-switched lasers are nanosecond pulse duration lasers with wavelengths efficiently absorbed by melanin. These include the frequency-doubled neodymium yttrium aluminum garnet (Nd:YAG), also known as the potassium titanyl phosphate (KTP) (532-nm) laser, the ruby (694-nm) laser, and alexandrite (755 nm) laser. Picosecond lasers are a more recently developed technology that may offer improved outcomes relative to Q-switched lasers. Currently available picosecond lasers include the 755-nm alexandrite and both a 532-nm and 1.064-nm Nd:YAG. Head-to-head clinical trials comparing nanosecond and picosecond lasers in treating solar lentigines suggest that picosecond lasers are more effective and carry a lower risk of post-inflammatory hyperpigmentation.
For patients with severely photodamaged arms, multiple modalities may be employed to produce the most optimal cosmetic result. As an example, IPL can be combined with one of the aforementioned fractionated dual wavelength lasers. For arms with diffuse dyschromia but otherwise mild photodamage, IPL can be followed by treatment with a Q-switched or picosecond pigment-targeting laser for discrete or low contrast lesions.
Erythema
Like the face, chronic photodamage on the arms can produce erythema, in addition to solar lentigines and mottled dyspigmentation. This erythema is usually the result of ectatic blood vessels and/or proliferation of angiomatous lesions. Patients with senile purpura, as may occur from anticoagulants and/or antiplatelet therapies, and patients with severe dermatoheliosis, will typically present with multiple thin ecchymoses and a history of easy bruising (Figure 3). Long-pulsed lasers, such as the 585-nm to 595-nm yellow-light pulsed dye laser, green-light KTP laser, and IPL are all effective at addressing these findings because they target hemoglobin via selective photothermolysis. In our practice in particular, we have had tremendous results with this mixed modality strategy. Because erythema is rarely seen as an isolated finding in patients seeking rejuvenation, we tend to treat first with IPL over the other modalities, owing to its being non-selective and capable of targeting both hemoglobin and melanin. Consequently, more reliable improvements in both erythema and pigmented lesions, like solar lentigines, can be achieved. Next, we treat with deep fractional lasers to restore the thicker and protective dermis, which seems to counteract the vascular fragility inherent to dermatoheliosis.
Skin Laxity
Owing to the same microstructural changes to dermal proteins that cause facial aging, the skin on the arms is subject to progressively worsening laxity as a result of both age-related and UV-induced degenerative changes to collagen, elastin and glycosaminoglycans. In recent years, a number of cosmetic treatments have been explored to combat the loss of elasticity and firmness on the upper arms that so often parallels increasing age. Desire for these treatments is also common among patients who develop more significant skin laxity as a consequence of significant fat reduction to the upper posterior arms, as occurs following liposuction.
Treatment options for skin laxity on the arms include radiofrequency (RF), ultrasound (US), and dilute and hyper-dilute dermal fillers (Figures 1 & 2). RF and US are technologies which primarily aim to tighten skin by way of delivering controlled thermal energy into the dermal and subdermal tissues. This induces immediate collagen denaturation and a contractile response, followed by a more prolonged phase of neocollagenesis and collagen remodeling. Consequently, RF and US have been shown to be modestly efficacious in tightening skin to patient satisfaction. The use of dilute and hyper-dilute dermal fillers, on the other hand, is predicated on a dual mechanism of action, which involves directly replacing lost volume as well as collagen biostimulation.
ThermageFLX (Thermage, Hayward, Calif) is a non-invasive and non-ablative RF device that delivers monopolar RF energy in the form of an electrical current. Through the inherent electrical resistance of dermal and subcutaneous tissue, heat is generated, which induces subtle damage to collagen. This, paired with an inflammatory cascade induced by the generated heat, produces the desired tightening effect. Though initially FDA cleared solely for the treatment of periorbital and lower face rhytides, regulatory clearance was granted in January 2006 for its use in off-face areas. In our experience, using lower energies and a higher number of passes is a protocol with improved efficacy, tolerability, and safety. As is the case when treating the face, the patient should always be evaluated for tightening and edema as endpoints that portend the desired cosmetic outcome. With respect to patient candidacy, RF devices such as ThermageFLX are unlikely to be of benefit to obese patients and patients with extreme skin redundancy. As it can be safely used in patients who have had prior cosmetic procedures, including laser surgery and dermal fillers, it is an appropriate modality for use in total arm rejuvenation, presuming the patient is otherwise deemed an appropriate candidate.
Thermistor-controlled subdermal monopolar radiofrequency (SMRF) (ThermiRF; Thermi Aesthetics, Irving, TX) is another RF skin tightening device capable of producing modest results. This technology continuously monitors epidermal surface temperatures with the use of an external infrared camera. Simultaneously, precisely controlled thermal energy is delivered to the deep dermal and subdermal plane through a thermistor-controlled radiofrequency probe. This allows for the maintenance of safe epidermal temperatures while subsurface collagen denaturation is ongoing. In a 2016 open-label, prospective trial involving 24 arms treated with SMRF, significant improvements in skin laxity were observed at days 30 and 90 after treatment.
Another choice for off-label skin tightening on the arms is ultrasound, of which there are two primary forms of delivery: microfocused ultrasound with visualization (MFU-V; Ulthera, Mesa, AZ), and high-intensity focused ultrasound (HIFU) (Doublo‐S; Hironic Co., Ltd). Both precisely heat the mid to deep subcutaneous layers without disrupting the papillary dermis and epidermis. Both also heat the deep dermis and fibromuscular layers, which includes the superficial fibroseptal network of the body, to between 60°C and 70°C. This is the optimal temperature for collagen denaturation and so induces collagen fibril contraction and immediate tissue tightening. It also triggers a wound healing response that perpetuates long-term neocollagenesis and neoelastinogenesis. Surface temperatures, on the other hand, remain between 45°C and 47°C during treatment in order to minimize unwanted epidermal injury.
Between the two technologies, MFU-V is more commonly used for cosmetic applications. Because of this, the vast majority of industry data on the efficacy of ultrasound for skin tightening is based on studies of MFU-V. A study by Alster and Tanzi treated six pairs of upper arms with single and dual-plane microfocused MFU-V (MFU-V; Ulthera, Mesa, AZ) and concluded all treated areas had improved between 3 and 6 months after treatment. Rokhsar and colleagues demonstrated the efficacy of MFU-V for the correction of elbow skin laxity. In this study, twenty patients received a single treatment of MFU-V 240 lines per arm. Of the sixteen available to be assessed 90 days after the procedure, 56% were found to have aesthetic improvement by blind investigators. It is important to note that, much like RF, obese patients and those with excessive skin laxity are not ideal candidates for MFU-V. The most significant and well-described limitation of MFU-V, which has been corroborated in our own practice, is pain and discomfort. It is for this reason that a thorough understanding of how to execute the procedure and use the ultrasound imaging transducer is critical, so as to minimize inadvertent targeting of tissues, such as bone.
Use of dermal fillers for off-face rejuvenation, including of the arms, has become increasingly popular for the treatment of skin laxity. Both hyaluronic acid (HA) and non-HA fillers, such as calcium hydroxylapatite [CaHA] (Radiesse®; Merz North America, Inc., Raleigh, NC, USA) and poly-L-lactic acid [PLLA] (Sculptra; Galderma Laboratories, L.P., Fort Worth, TX) can be used for this indication. However, non-HA fillers may offer greater and longer-lasting improvements in the upper arm area because they may have comparatively greater collagen biostimulation, which regenerates skin to provide long-lasting elasticity and firmness. The ability of CaHA microspheres to stimulate the production of collagen has been shown in multiple studies, including this author’s work in 2004 using electron microscopic quantification of neocollagenesis and neoelastogenesis (Marmur ES, Phelps R, Goldberg DJ. Clinical, histo-logic and electron microscopic findings after injection of a calcium hydroxylapatite filler. J Cosmet Laser Ther. 2004;6:223) and results from a histiocytic and fibroblastic response that serves as a scaffold for collagen and elastin formation. Neocollagenesis in response to PLLA, on the other hand, appears to result from a mild-to-moderate foreign body-type reaction.
Although typically suited for supraperiosteal, subdermal, and deep-dermal placement, CaHA and PLLA can be diluted for the purpose of injection more superficially for dermal rejuvenation. This is, in part, because superficial injection of less dilute concentrations can lead to undesirable product visibility. There are, of course, important differences for the injector to consider with respect to dilution parameters and injection technique, and these are dependent on choice of filler.
Diluted CaHA is generally defined as reconstitution with lidocaine or saline using ratios of 1:1, whereas hyper-diluted CaHA refers to reconstitution using ratios of 1:2 or higher. For treatment of the upper arms, the recommended dilution for CaHA, in most cases, is 1:2. In select situations and in individuals with thicker skin, however, dilution ratios of 1:1 may be more appropriate. Volumes of 3mL per arm are usually required. To dilute properly, the syringe containing original CaHA is connected to a LuerLock syringe containing diluent via a female transfer adaptor. It is important that both syringes are large enough to accommodate the combined volume of filler and diluent. We recommend at least 20 passes between syringes to ensure sufficient mixture of the two. Injection technique and choice between needle and cannula are largely injector dependent. Regarding technique for the upper arms, we tend to favor fanning in the immediate subdermal plane. With respect to treatment number, the consensus recommendation is to assess the patient 3- to 4-months post-injection for response and to re-inject as necessary thereafter. In our experience, 3 to 4 sessions are usually required within the first year after treatment. The patient should be counseled to expect the need for maintenance injections at a frequency of approximately every 12 to 18 months thereafter. It is also important to note that results may not be seen for 6 months or longer, particularly in older patients over the age of 50.
Higher dilutions are required when injecting PLLA and concentrations range by injector preference. Six to 36 hours prior to injection, PLLA is diluted in distilled water and combined with anesthetic, which may or may not include a vasoconstrictive agent. Unlike for CaHA, there is no established consensus guideline for PLLA injection into non-facial areas, thus, techniques used in the literature are quite variable. Volume of product used typically ranges from 4.5 to 8mL (average = 6mL) and the most widely used technique is retrograde injection at the level of the deep dermis or subcutaneous layer. Approximately 0.05-0.1mL is placed per injection. Some injectors favor the use of microcannulas, which allows access to deeper planes with lower incidence of hematomas and less discomfort. As for PLLA injection in the face, massaging the area is absolutely critical at the end of each session. Subcutaneous nodules remain the most common side effect. Risk of this can be reduced by using lower concentrations, injecting into the subcutaneous plane and vigorous massage both in office and at home. Improvement in skin laxity can often be seen as early as 6 to 8 weeks after the first session, with results lasting for up to 2 years.
Our preferred approach to PLLA for the upper arms is as follows. The product is reconstituted the day prior to injection with 8mL of sterile distilled water and is kept at room temperature until time of treatment. Immediately prior to injection, the vial is shaken vigorously to the point of homogenization. Separately, 12mL of aqueous solution is prepared by combining 8mL of distilled water and 4mL of 2% plain lidocaine. When volumes of vial and solution are combined, this results in a final PLLA dilution of 20mL per vial. A 1mL Luer-lock syringe is then used to aspirate 0.4mL of product and 0.6mL of solution and these two volumes are mixed together. This 1mL volume of diluted PLLA is then injected in linear retrograde fashion, injecting approximately 0.05mL into the deep dermis in parallel, stopping when the entire desired area is treated. This approximates to 4-6mL per arm. We then perform vigorous massage in the treated area for 10 minutes and instruct patients to use the same technique at home, twice per day for a duration of 10 days. We repeat treatments at a frequency of every 4 weeks for 2-4 sessions, depending on response.
Excess Adiposity
Excess adiposity, particularly on the upper posterior aspects of the arms, is a common and increasingly frequent concern with age as a result of a variety of factors. Treatment of excess adiposity can be done with both invasive and non-invasive measures. Of the non-invasive measures, the most effective is cryolipolysis (CoolSculpt; Zeltiq Aesthetics, Pleasanton, CA). When there is a large amount of excess upper arm adiposity, traditional liposuction with or without fat graft contouring is generally preferred.
The suggested mechanism of cryolipolysis is cooling-induced lobular panniculitis, which induces an inflammatory response that promotes cell macrophagy over time. During the procedure, an applicator is placed on the treated area to extract heat gradually until the target temperature (−10°C to −1°C) is reached. This temperature is then sustained for a predetermined period of time. Intracellular lipids are subsequently metabolized and eliminated by the body, typically within 4 months post-procedure. Adipocyte apoptosis has also been shown to increase collagen content within adipose tissue. The combined result of these effects is an overall reduction in fat layer thickness of up to 20%–26% in the treated area. A 2015 prospective study on the use of cryolipolysis for the treatment of excess arm and inner thigh adiposity found the treatment to be effective overall. In this study, which treated 10 arms and 24 inner thighs, found a combined 0.41-cm and 0.72-cm circumferential reduction after a single treatment session at the 3 and 6 month follow-ups, respectively. Notably, specific analysis was not performed on the arms-only group. However, the data suggest cryolipolysis can be a safe and effective treatment of excess arm adiposity.
When a large amount of adipose tissue must be removed, liposuction, either suction-assisted or laser-assisted, is often more appropriate. Suction-assisted, or conventional, liposuction refers to the removal of localized areas of fat by suction through a cannula. Though incredibly popular, it is associated with long procedure duration, blood loss, swelling, bruising and operator fatigue. Laser-assisted liposuction was created to circumvent these limitations and involves the use of a laser fiber prior to suction removal. The original purpose of the laser was to circumvent the need to rely on the mechanical trauma produced by back-and-forth cannula movements. Rather, lipolysis is attained by direct light and heat, which correlates to greater hemostasis and lower rates of blood loss, swelling, bruising and intraoperative pain.
An additional advantage of laser lipolysis is contraction and overall skin shrinkage, and it is for this reason that we frequently prefer this approach for patients we deem appropriate candidates for liposuction. This was first shown in 2002 in a study using a 1064-nm Nd:YAG laser to treat flaccid areas of skin in 245 patients. During the procedure, laser energy was delivered via cannula and a fiber was introduced through a 2- to 3-mm incision. As the authors expected, the procedure was found to be less traumatic than traditional liposuction, which they attributed to the small 1mm cannula diameter and reliance on laser energy, rather than mechanical trauma, for adipocyte injury. A more unexpected finding was that the thermal effects of the laser produced skin retraction and collagen remodeling, allowing the authors to conclude that laser lipolysis offered this clear advantage over traditional liposuction. This was subsequently supported histologically by Goldman et al. in a study involving treatment of the necks and jowls of 82 patients with laser-assisted liposuction using a 1064-nm Nd:YAG laser. In addition to ruptured adipocyte membranes, histological studies showed coagulation of collagen and small blood vessels and clinical evaluation demonstrated contraction of cervicofacial skin, suggesting the 1064-nm Nd:YAG laser caused new collagen synthesis.
A more recent development in laser-assisted liposuction has been dual wavelength technology for additional cosmetic benefit. These revolutionary laser lipolysis devices combine a 1,064nm Nd:YAG laser with a 1,319nm infrared Nd:YAG laser (ALLURA; Sciton, Inc., Palo Alto, CA) and have demonstrated considerable success among our patients. The potential implications of this dual wavelength system were first shown by Dang et al. in a study which investigated the impact of each wavelength on collagen synthesis. The authors demonstrated that mouse skin irradiated with a 1,064nm Q-switched laser increased synthesis of collagen type III, whereas long-pulsed 1,320nm produced a greater increase in collagen type I, a difference that was attributed to variable photothermal effects on irradiated tissue. This was the first study to show that the combination of a 1,064nm and 1,320nm wavelength induces a greater degree of collagen synthesis than either wavelength alone. Years later, the clinical significance of these findings was solidified in a study that found the same dual-wavelength combination produced a 26% improvement in skin elasticity and a 17% reduction in skin area, allowing the authors to conclude that it was capable of shrinking and tightening skin.
The rationale behind the two chosen wavelengths in the 1,064nm / 1,319 Nd:YAG system (ALLURA; Sciton, Inc., Palo Alto, CA) used in our practice is the following: the 1,064nm wavelength is an efficient wavelength for lipolysis which preferentially destroys the highly vascular superficial fatty layer. It is also better absorbed by oxyhemoglobin, a property that allows it to produce a greater degree of thermal energy and, consequently, improve hemostasis. In contrast, owing to its greater affinity for water and lower scattering in fat, the thermal energy generated by the 1,319nm wavelength remains confined to the area just beyond the tip of the fiber. Consequently, the 1,319nm wavelength preferentially damages collagen in fibrous septae, a precursor to tissue retraction.
Patient Assessment & Selection
In our busy practice we routinely take extra time during cosmetic consultations to ask about concerns such as arms, abdomen, buttocks, flanks, leg veins, or anything else they have in mind. This open-ended approach often intrigues patients to question what else CAN be done. Lasers or devices are our #1 most popular treatment category for arms. Once the skin tone and appearance has been discussed, patients address areas of excess wrinkling, commenting that when they work out or wear sleeveless clothing they especially notice certain areas. Here we discuss surgery, which we do not offer, or fillers, which give instant gratification at a low risk.
Patient assessment for fillers is slightly more involved than lasers, which have been covered extensively elsewhere. For arms, patients with mild to moderate laxity and good dermal thickness are ideal candidates. Those patients with very fine, thin skin in the setting of sarcopenia and osteopenia present a challenge because they need high volume filler that spreads evenly without forming nodules but that provides volume. Most of our arm rejuvenation patients are well established in our practice and have already experienced some form of cosmetic surgery on their face or even knees. Also, most of our arm filler patients are quite fit with low body mass index and exercise frequently. Finally, patients with liposuction defects or depressed scars are ideal candidates for arm rejuvenation using this combination therapy approach. Potential contraindications for arm filler and rejuvenation include active autoimmune diseases (SLE, CREST, DM,) history of chronic pain or vascular disease in the arm, lymphedema of the arm post lymphadenectomy, scarring with large surface areas or contractions especially when crossing over the joint, allergies to ingredients in the filler(s) of choice, and patients with unrealistic expectations or who are historically unsatisfied with cosmetic results.
Creating a Master Plan
Creating a Master Plan is a key to success in all cosmetic surgery. This is especially true for treatment of the arms which require more patient education and patience as the final result may require a series of sessions. We provide two forms of a Master Plan for all patients and recreate both forms at almost every visit given that the plan is organic and changes with the patient’s needs and feedback. Each practice must have their own similar forms that optimize their workflow, medical records, billing, and medicolegal operations. They do not replace consent forms and yet are vital reference points and protective in the event of a dispute or misunderstanding.
The first of the two forms of our master plan is an illustrated personalized plan. This might include important information on the margin such as the date of an upcoming life event (wedding, reunion, etc) plus a strategic calendar of procedures leading up to that event. Patients appreciate a clear timeline of what will be done and when on their master plan.
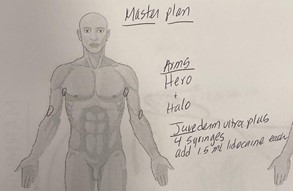
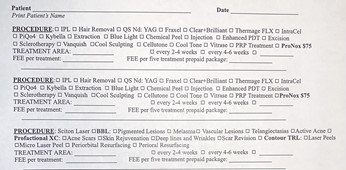
The second form is a financial consent form. While ours is not fancy, it makes it easy for us to customize. We do not have one price per area per procedure printed on this form. Instead, we have procedure names and a space for prices for one or multiple areas where we show the a la carte versus bundles with a generously discounted fee when all are done at one visit. For arms, it is helpful to bundle skin tightening, filler, and resurfacing all in one visit for the ideal triad of deep tissue, volume, and more superficial skin treatment. And for the arms, the ideal plan usually requires a series of these bundled treatments. Always take the time to document how many treatments, how often, with whom, the price per session, and the estimated range of improvement expected. For example, IPL, forearms only, $495 per session with an RN, 3-5 sessions, 40-80% improvement expected but with likely irregular pigment for the first 3 sessions; best to combine with fractional laser for more even results and better skin integrity, highly recommend sun protection and healing serum . As always, setting clear expectations in writing is very helpful for all.
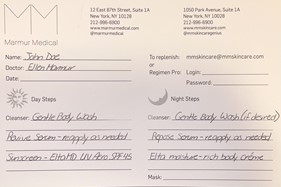
Patients are given to take home a folder with these personalized master plans and financial consent forms, both of which are signed and dated by the patient. The plans are scanned into their electronic medical records and valid for three months. We recommend including an information email address on these forms for patients to have easy access to your patient coordinators as they have questions about their master plans. Most of our patients complete the first step of their treatment plan on the same day as the consultation. We have them return for follow-up in 3-4 weeks for their second session during which time we offer a free laser treatment for any bruises, which are commonly due to small venous bleeding and are not considered to be serious adverse events. Some patients are instructed to gently massage and press areas of swelling to ensure even distribution of the filler. All laser and filler patients are provided with a skincare master plan as well, with personalized instructions for specially formulated aloe-based serums and a home LED device to optimize results.
Case Descriptions
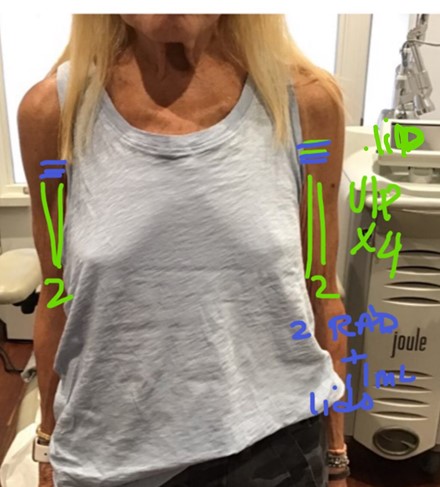
#1) S.S.: Patient presented as a Fitzpatrick Type I, 74 year-old female with the desire to improve the texture of her upper arms. Patient is hypermetabolic, works out daily with weights, is post-menopausal with low bone density, low body fat, and has severe sun damage. The patient was treated with four syringes of Juvederm Ultra Plus dermal fillers and two syringes of Radiesse (calcium hydroxylapatite) with 1.0 mL 1% lidocaine with epinephrine in one session.
#2) A.C.: Patient presented as a Fitzpatrick Type I, 61 year-old female with a complaint of thin skin and laxity of the upper medial arms. Patient is extremely athletic and has a low BMI. Patient’s arms were treated with two vials of poly-L-lactic acid (Sculptra) injectable reconstituted as directed according to the package insert with 5 mL of bacteriostatic water plus an additional 4mL of 1% lidocaine without epinephrine and non-buffered in one session. The injection technique was as follows: after desired reconstitution, using a 23g needle, tent up the skin to provide a space above the brachial veins and ulnar nerve, inject the needle to the desired depth, draw back with reverse pressure to ensure no blood in needle, and slowly inject the PLLA with a long fanning technique both anterograde and retrograde watching closely for a pain reflex (indicating close proximity to vein, nerve, or artery) or bruising. Fill to the desired smooth endpoint and gently smooth or massage the injectate to intersperse naturally in the soft tissue. No massage is needed after the visit. The patient returned in 3 months and 6 months and did not require further injections and was happy with the continued results.
#3) S.F.: Patient presented as a Fitzpatrick Type I, 51 year-old female with chronic severe ecchymoses and a complaint of fragile and easily-bruising skin on the arms upper and lower arms. The patient wanted to improve her skin’s integrity and barrier strength, as well as minimize the likelihood of bruising very easily in the future. At her suggestion, the patient was treated with a series of six (6) Fraxel Dual Restore laser resurfacing treatments over the course of 23 months. The first three treatments were completed within intervals of one month, and the last three treatments were completed within intervals of merely three weeks. The following is a testimonial from the patient, received via e-mail communication:
“Even if you can’t see it in these pics, my forearm skin is just far less likely to tear, bleed and bruise than it was before. The pre-Fraxel pic with bruises/bleeding was just from regular scratching.. that just doesn’t happen anymore (even if I scratch really hard.) I’ve actually noticed the most meaningful improvement & reduction in bruising/bleeding & fragile skin since the last treatment or two. Forearms are dramatically improved from the bruising/bleeding fragile skin start.” (S. F., personal communication, March 23-24, 2021).
It is apparent, through the photos as well as the patient’s testimonial, that she was extremely pleased as well as satisfied with her results.
#4) K.K.: Patient presented as a Fitzpatrick type II, 49 year-old female with complaints of severe photodamage and benign guttate hypomelanosis on the upper arms. Patient is an ultra- marathoner for years and always had a low BMI. The patient was treated with ten (10) Fraxel Dual Restore laser resurfacing treatments, two (2) Sciton Joule laser resurfacing treatments, and one (1) BBL (broadband light) treatment to address the hypopigmentation and improve the tone of the skin. The Fraxel Dual Restore treatments were done over the span of 6.5 years, with average intervals of 7.5 months between treatments. The two Sciton Joule treatments were completed at one 5-month interval. The BBL treatment was completed one month after the first Sciton Joule treatment.
#5) S.Z.: Patient presented as a Fitzpatrick Type II, 64 year-old male with a complaint of hyperpigmentation on his arms caused by decades of sun exposure. Patient enjoys the outdoors and tans with ease. The patient was treated with two (2) BBL (broadband light) treatments over the span of two months. The first treatment was done at the beginning of February 2021 and a 10% improvement was noted. The second and last treatment took place at the beginning of March 2021, which cleared the leftover pigmentation. Patient declined a third treatment as he was satisfied with his results.
Conclusion
Patients want younger appearing arms with more clear and firm skin. Arm rejuvenation by cosmetic surgeons can be performed using many of the same devices and injectables as with the arms, face, chest, legs, and other areas of the body but with new treatment techniques. Applying our knowledge of the unique anatomy and function of the arms with the techniques we know so well on the other areas of the body and face is an obvious extension of cosmetic surgery. As with every new frontier in medicine, learning the nuances and erring on the side of minimal to moderate goals in the name of safety is especially important with arm rejuvenation. It will be interesting to see how repurposing our current technologies will induce the invention of exciting clinical advances with new, more specific treatments for arm rejuvenation.
Images
Figure #1: S.S.
Before & 7 Months Later:


Method: Patient was treated with 4 syringes of Juvederm Ultra Plus and 2 syringes of Radiesse plus 1.0 mL 1% lidocaine with epinephrine.
Figure #2: A.C-H.
Before and 10 months after:


Method: Patient was treated with 2 vials of Sculptra.
Figure #3: S.F.
Before and After: